Age-Related Macular Degeneration (AMD) is a deterioration of the retina and choroid that leads to a substantial loss in visual acuity (sharpness of vision). AMD is the leading cause of significant visual acuity loss in people over age 50 in developed countries.
Causes: The exact cause of AMD is unknown, but the condition develops as the eye ages.
There are 2 types of AMD: non-neovascular or dry AMD; and neovascular or wet AMD.
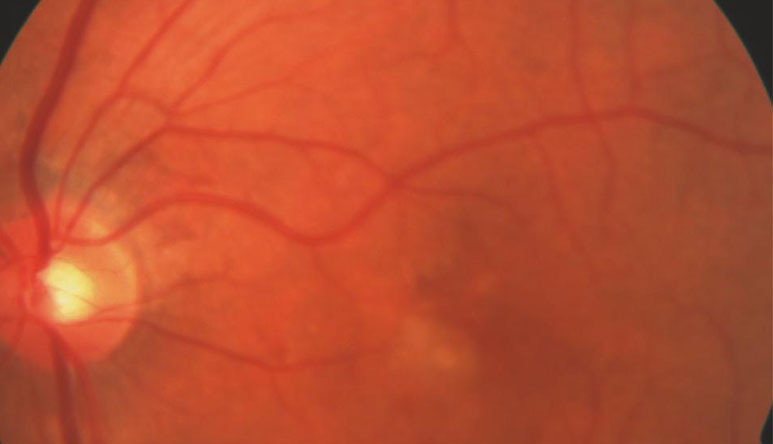
In early stages of dry AMD, the hallmark is drusen—pale yellow lesions formed beneath the retina (Figure 1A). Drusen are usually harmless, but as they accumulate, dry AMD can progress. Atrophic areas (areas of atrophy or wasting) in the retina also may develop; if the atrophic area is significant and with sharp borders, it is termed geographic atrophy (GA) (Figure 1B).
Figure 1:
Dry AMD ( Age-Related Macular Degeneration).
A. Drusen (indicated by arrow).
B. Geographic atrophy
Photo courtesy
Anat Loewenstein, MD
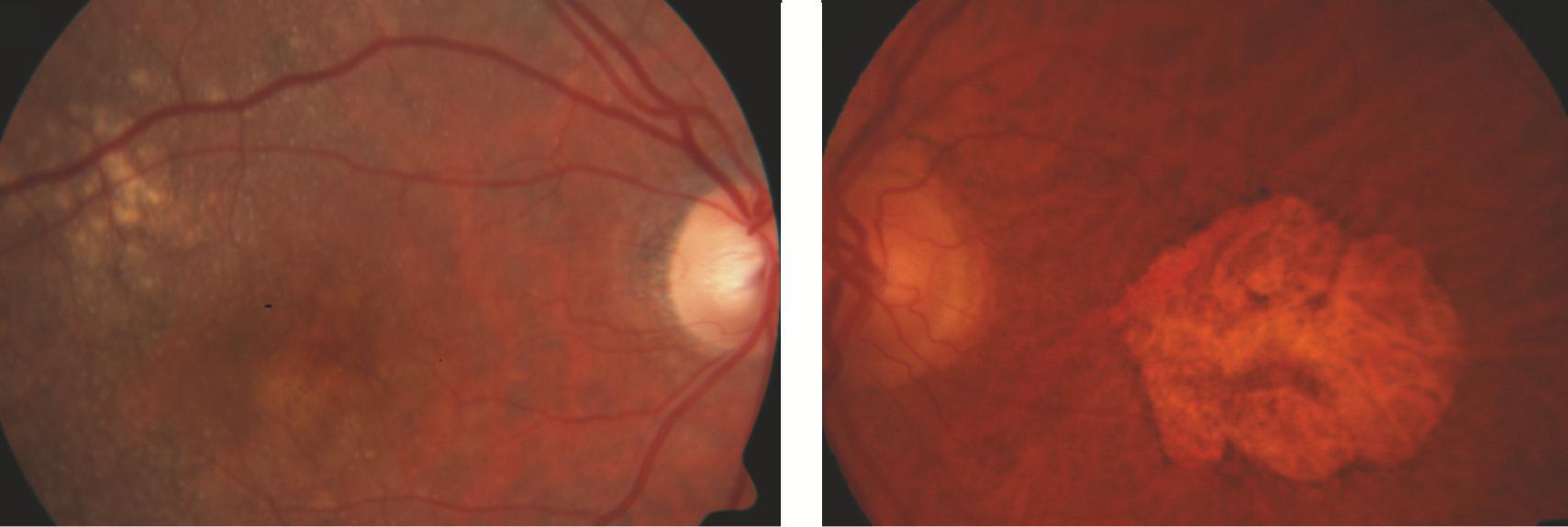
GA is the advanced form of dry AMD, which may be associated with loss of central vision.
In wet AMD (Age-Related Macular Degeneration ), there is a sudden or gradual decrease in visual acuity, blind spots in the center of vision, and distortion of straight lines. The hallmark of wet AMD is choroidal neovascularization (CNV) (Figure 2).
CNV occurs when abnormal blood vessels grow beneath the retina; these can bleed or leak and cause a distortion of the retina’s structure. Ultimately, the CNV can turn into a disciform scar that replaces the normal architecture of the outer retina and leads to permanent loss of central vision.
Figure 2
Wet AMD (Age-Related Macular Degeneration). Choroidal neovascularization (indicated by arrow).
Photo courtesy Anat Loewenstein, MD ( Macular Degeneration)
Risk Factors:
• Age—the strongest risk factor • Family history of AMD
• Caucasian race • Cigarette smoking
Possible risk factors:
• Female gender • High cholesterol
• Lower level of education • Sunlight exposure
• Light iris color • Low dietary fish intake
• Far-sightedness • Higher body mass index (BMI)
• Cardiovascular (heart) disease • Having a diet low in lutein and
• High blood pressure zeaxanthin/antioxidants
Diagnostic Testing: Disease features related to AMD may be found in the retina and in the layers beneath it. According to these abnormal findings, AMD is classified as dry or wet. An AMD diagnosis is made by a clinical examination with a slit lamp and by using several types of imaging, including:
• Fluorescein angiography (FA)
• Indocyanine green angiography (ICGA)
• Optical coherence tomography (OCT)
• Optical coherence tomography
angiography (OCTA)
WHAT IS THE RETINA?
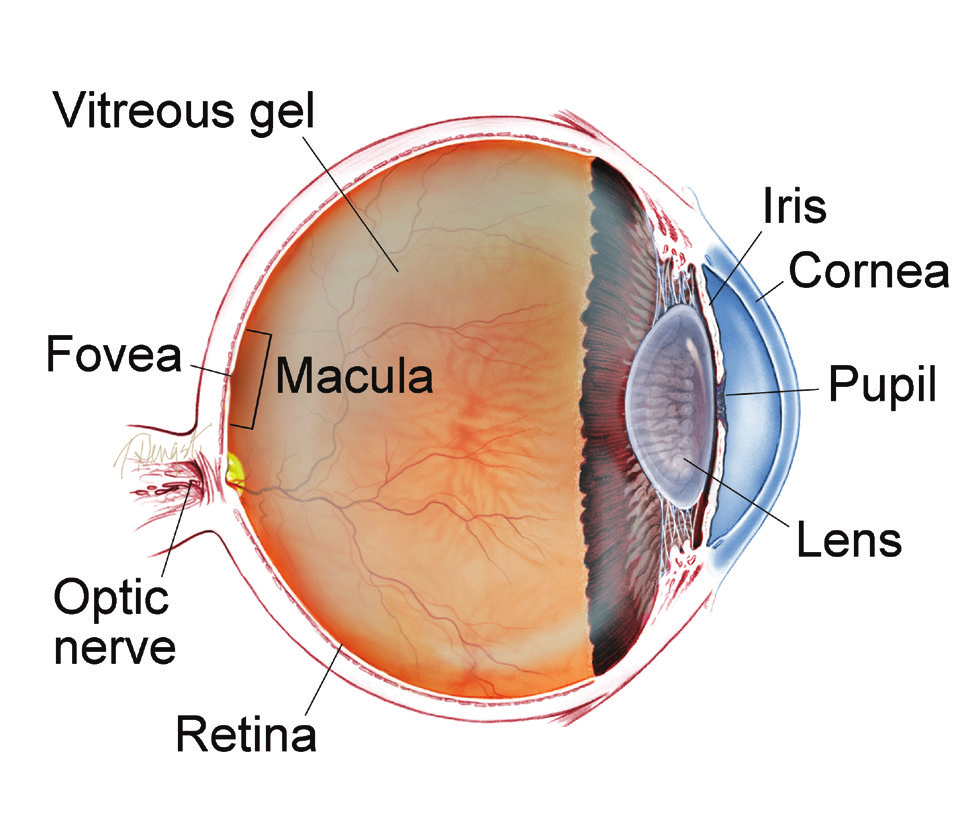
THE RETINA is a thin layer of light-sensitive nerve tissue that lines the back of the eye (or vitreous) cavity. When light enters the eye, it passes through the iris to the retina where images are focused and converted to electrical impulses that are carried by the optic nerve to the brain resulting in sight.
Treatment and Prognosis: Wet-AMD treatment has been revolutionized in recent years after the discovery of vascular endothelial growth factor (VEGF), a family of compounds in the body. VEGF regulates the growth of abnormal new blood vessels
in the eye — known as neovascularization — that can lead to wet AMD.
Anti-VEGF drugs have been developed to help stop neovascularization and preserve vision for AMD patients. There are currently
4 anti-VEGF drugs:
• Avastin® (bevacizumab)
• Lucentis® (ranibizumab)
• Eylea® (aflibercept)
• Beovu® (brolucizumab)
Wet AMD cannot be cured, but its progression may be blocked with the use of intravitreal (in-the-eye) anti-VEGF injections. These injections may preserve, and even recover, vision. Local anesthetic eye drops are given before the injections to numb the eye and minimize discomfort.
SYMPTOMS
In early stages, AMD may have no symptoms at all. When the disease progresses, the symptoms are:
• Distortion (warping) of straight lines
• A decrease in the intensity or brightness of colors
As the macular degeneration progresses, AMD symptoms include:
• A gradual or sudden loss of central vision, or
• Dark, blurry areas in the center of vision
There are 3 anti-VEGF treatment regimens commonly used. The
best option is chosen in consultation with your retina specialist.
1. Pro re nata (PRN) or “treat and observe”—patients are treated
with three initial monthly injections, followed by treatment
as needed.
2. “Treat and extend”—after 3 initial monthly injections, the time
between treatments is gradually increased as tolerated. Some
eyes will continue to require monthly injections, but others can
be treated less often as long as the wet AMD is controlled.
3. Monthly injections.
Before the first anti-VEGF drugs were introduced, wet-AMD patients were
treated with laser photocoagulation or photodynamic therapy (PDT).
Anti-VEGF drugs have greatly improved wet-AMD treatment
since 2005; patients today have a much better chance of maintaining
their central vision so they can read, drive, recognize faces, and live
normal lives.
No current treatment can prevent visual loss for patients with
GA (the advanced form of dry AMD). However, the Age-Related Eye
Disease Studies (AREDS), conducted by the National Eye Institute,
have found that a nutritional supplement formula (AREDS-2
supplement) may delay and prevent intermediate dry AMD from
moving to the advanced form.
The AREDS-2 supplement formula, which is widely available over
the counter, contains specific doses of vitamins and minerals used
in the AREDS-2 Study:
• Vitamin C • Lutein
• Vitamin E • Zeaxanthin
• Zinc
Although patients with either form of AMD can experience
a severe decrease in visual acuity, they will almost never be
completely blind.
Choroid (pronounced CORE oid): The layer of blood vessels and connective tissue between the retina and the white of the eye, also known as the sclera.
Choroidal Neovascularization (CNV): Growth of abnormal new blood vessels in the choroid layer of the eye that grow under the retina and macula and disrupt vision.
Disciform scar: A scar that develops in the macula area of the retina resulting from leakage and bleeding from abnormal blood vessels (neovascularization) in the eye.
Fluorescein angiography (FA): An imaging technique where a yellow dye called sodium fluorescein is injected into a vein in the arm, allowing a special camera to record circulation in the retina and choroid in the back of the eye. This test can be very useful in diagnosing a number of retinal disorders.
Indocyanine green angiography (ICGA):
A diagnostic procedure that uses a green dye to illuminate blood flow in the choroid, which is a layer of blood vessels located between the white of the eye (sclera) and the retina that supplies nutrients to the inner eye.
Laser photocoagulation: A surgical technique that uses a highly targeted laser light to seal blood vessels and coagulate (clot) tissue.
Optical coherence tomography (OCT): A noninvasive imaging technique that uses light to create a 3-dimensional image of your eye for physician evaluation.
Optical coherence tomography angiography
(OCTA): A noninvasive imaging technique that uses light to image the blood vessels in different layers of the retina and choroid.
Photodynamic therapy (PDT): A treatment for macular degeneration in which a light-activated medicine (verteporfin) is injected into the bloodstream followed by application of a cold laser which targets abnormal blood vessels growing in the macula at the center of the retina.
Slit lamp: An instrument that combines a highintensity light source with a microscope to examine the external and internal structures of the eye, including the optic nerve and retina.
Bibliography
THANK YOU TO THE AUTHORS
Sophie J. Bakri, MD Audina Berrocal, MD
Thomas Ciulla, MD, MBA Geoffrey G. Emerson, MD, PhD Roger A. Goldberg, MD, MBA Dilraj Grewal, MD
Larry Halperin, MD Vi S. Hau, MD, PhD
G. Baker Hubbard, MD Talia R. Kaden, MD
M. Ali Khan, MD
Mathew J. MacCumber, MD, PhD Timothy G. Murray, MD, MBA Oded Ohana, MD, MBA Jonathan L. Prenner, MD
Carl D. Regillo, MD, FACS Naryan Sabherwal, MD Sherveen Salek, MD Andrew P. Schachat, MD Michael Seider, MD
Janet S. Sunness, MD Edward Uchiyama, MD Allen Z. Verne, MD Christina Y. Weng, MD, MBA Yoshihiro Yonekawa, MD
EDIT OR
John T. Thompson, MD
MEDICAL ILL US TRAT OR
Tim Hengst
Copyright © The Foundation American Society of Retina Specialists
Committed to improving the quality of life of all people with retinal disease.